General Medicine elog 3
Hi ,I am Swetha 3 rd semester student.This is an online elog book to discuss our patient health data after taking his consent.this also reflect my patient centered online learning portfolio.
Chief complaints : A 62 year old male patient ,toddy tree climber by occupation,resident of Nagaram ,came with complaints of decreased urinary output,loss of appetite , vomitings , shortness of breath.
HOPI: Patient was apparently normal 4 years back,then he developed weakness and pain of limbs backpain and used on medication, following which pain didn't subsided took MRI spine and told to have decreased bone density and used painkillers onces a day for 3-4 year and also he was diagnosed with hypertension and on regular antihypertensive .since than he had pedal edema and occassional SOB on excretion and on medication .
Since 1 week patient has loos of appetite , vomiting weakness and decreased urinary output.No history of burning micturition.cough cold fever .
Covid vaccination is done .
Past history : no significant history .no history of any surgery
Person history : loss of appetite,non vegetarian diet . irregular bowels, decreased urinary output , alcoholic(occasional) and smoking since 40 years .no history of known allergies.
Family history:no history of diabetes, hypertension,heart disease, stroke,cancer,TB, asthma
Systemic examination:
CVS : ,cardiac sounds present ,no thrills cardiac murmur
Respiratory system: dyspnea present ,no wheeze position of trachea is central, vesicular breath sounds present
Abdomen : scaphoid shape of abdomen, no tenderness no palpable mass,no free fluid ,not palpable liver spleen bowel sounds present.
CNS : conscious, coherent, cooperative speech is normal.
Investigation:
Diagnosis
AKI on CKD , polycystic kidney disease ,HTN and supra umbilical hernia
On dialysis
Treatment:
T.lasix 40mg /po/BD
T.noddsis500 mg /po/BD
T.shelcal 500 mg /po/ BD
T.MVT po/OD
Salt and fluid restrictions
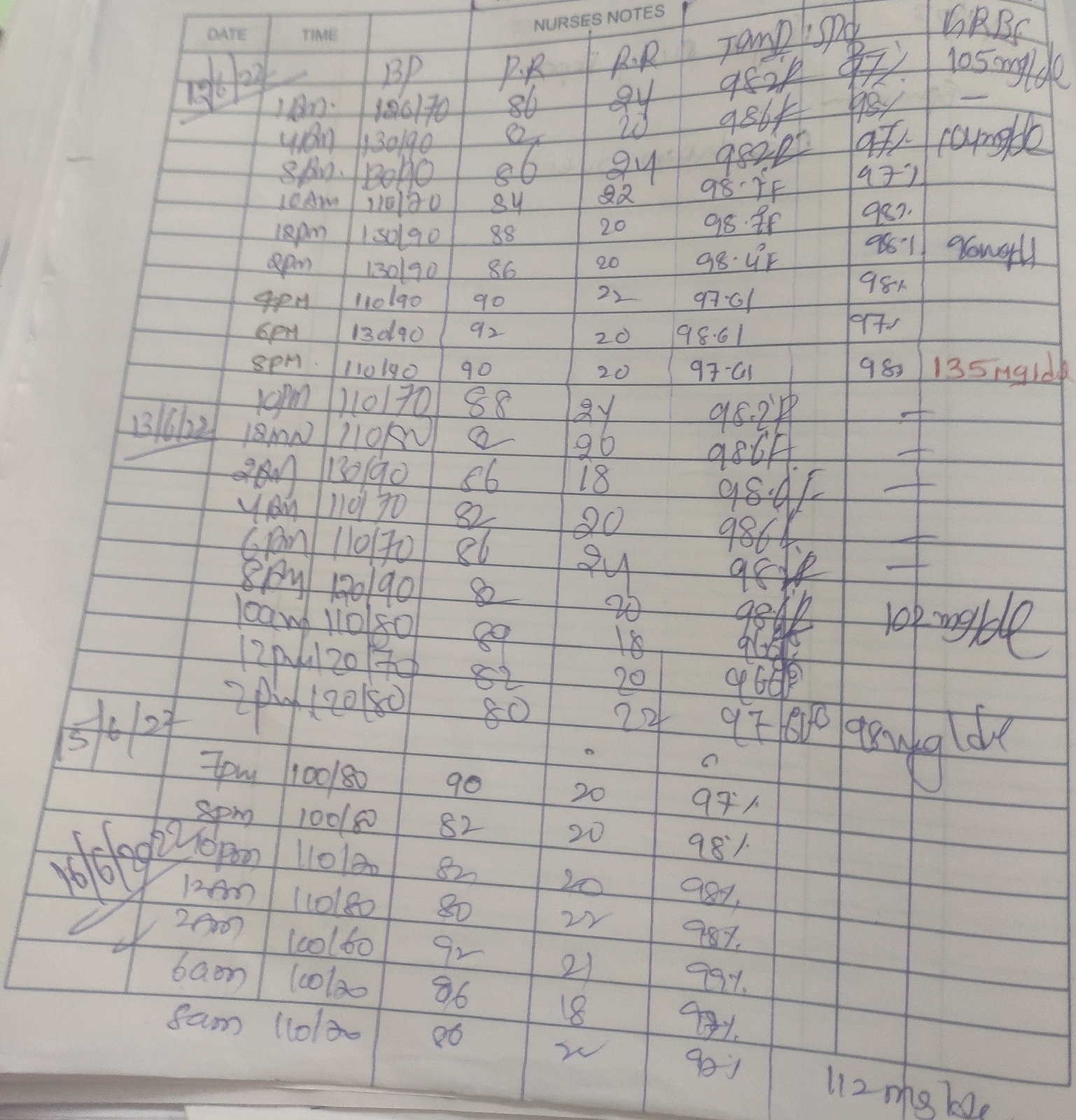
BP/PR/Temp every 4 th hourly
GRBS every 12 hourly
Inj: lasix 40 mg .iv